What Niger's AMR outbreak means for the world
In this edition of The Naked Scientists, why we need to pay closer attention to antimicrobial resistance in some of the world’s poorest nations...
In this episode

00:46 - What is behind the AMR outbreak in Niger?
What is behind the AMR outbreak in Niger?
Kirsty Sands, University of Oxford
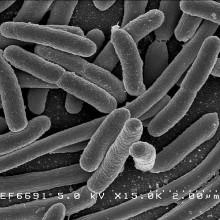
Researchers are tracking a worrying rise in antimicrobial resistance - or AMR - in Niger. A new study has shown that poor sanitation, malnutrition and an overburdened healthcare system, has fuelled the spread of a highly resistant form of E.coli in the West African state, and it’s hitting young children the hardest. Experts are also concerned that current war-torn regions, such as Gaza, are also ideal breeding grounds for antimicrobial resistance to flourish. First, let’s hear from Kirsty Sands at Oxford University about what she found has happened in Niger, a country currently in the world’s top ten per cent of countries plagued by antibiotic resistance…
Kirsty - So currently in Niger there are large numbers of children that are severely malnourished. In hospital facilities in Niger, resources are extremely limited, so many children are admitted into quite confined spaces. If these children are exposed to bacteria that may be present in the clinical environment or can be transferred between patients and visitors, there is a greater risk that these children may pick up these bacteria. We previously screened over 6,000 hospital surfaces and in doing so we found a huge diversity of drug-resistant bacteria colonising different surfaces throughout the ward.
Chris - Why, given that's thousands of miles away, do we need to be paying attention?
Kirsty - Of course the burden is highest in environments where there are such limited resources. However, when you look at the global scale, we do see the same bacteria, these same high-risk clones, being found - maybe in smaller numbers - but as we know, people are travelling across the globe. We see bacteria spreading through borders, through people, food, and the environment. And that's why surveillance projects like ours matter. They give us this ability to detect emerging threats and try to understand what the current bacterial landscape is like.
Chris - And is there evidence that when these resistant forms pop up in new geographies, like London for example, they actually cause a problem?
Kirsty - Yes, absolutely. We often consider hospitals as a hotspot and these are places that can fuel the growth and spread of bacteria. And of course, if you are a patient in a hospital in London and you become colonised with a multi-drug-resistant bacteria, you may then go on to become infected with the same bacteria. Because it's drug-resistant, the antibiotics that may be given are likely to be ineffective, may increase length of hospital stay, and just complicate recovery.
What is antimicrobial resistance?
Brad Spiller, Cardiff University
What do we need to know about the threat posed by AMR? Brad Spiller is head of medical microbiology at Cardiff University…
Brad - I like to think about bacteria as a supervillain. In the theatres it was the Avengers, where you had Thanos. Thanos is the giant purple bacteria and he's running around collecting the infinity stones. And the infinity stones are the equivalent of the resistance genes, right? So as he gets each individual stone, he gains a new power and he becomes less and less killable. The O'Neill report that was commissioned by the UK government said that by the year 2050, more people are going to die from antibiotic or antimicrobial-resistant bacteria than die from cancer and diabetes combined. And I mean, that's a scary number - that's like 10 million people a year.
Chris - How does this arise? When I was first a doctor, for example, the card that the microbiologist in my hospital gave me for what drug to use for which infection - when I looked at that the other day, none of those drugs work anymore. When we look at those sorts of infections, I couldn't use those drugs today. Why have we ended up in that position and how?
Brad - When penicillin was discovered in 1928 by Alexander Fleming, there were already a few bacteria in the wild that carried natural resistance. The resistance has always been there - it was just sort of at low levels. What antimicrobial resistance is, is actually that selection process. So when we use an antibiotic, it kills the sensitive bacteria and it selects the tough ones. So those survivors multiply and pass that resistance on. That resistance can be a DNA mutation. Often it's actually on a small extra DNA loop called a plasmid that the bacteria can share between them. Antibiotic overuse and misuse, plus heavy antibiotic use in things like agriculture, accelerate that selection. The real danger is when you get a single strain that collects resistances to multiple drug classes. Penicillin is the oldest one, and the reason that we have probably more penicillin resistance than anything else is because we've been using it longer. Tetracyclines came along in the '60s. And there are some, like Group B Streptococcus, for instance, greater than 95% of them are resistant because in the 1960s they used tetracycline for everything. To some degree, that's part of the problem we have now. People try to use antibiotics to cure a cold - which has no effect whatsoever on a virus. And all you're doing is basically giving that selection process and getting rid of the bacteria that we could have an effect on.
Chris - In other words, if you go out into the environment, your chances of running into a microbe that now has resistance against the antibiotic shoots up because we've used a lot of that antibiotic. So that if you're going to get that bacterium, you're going to get one that's resistant just because there’s so many of them around now, because we've killed all the ones that were sensitive.
Brad - Yes, it's that pressure - the overuse and misuse. The other thing is taking the antibiotics through the whole course. You might start to feel better and stop taking the antibiotics, but that's exactly the sort of thing that drives mutation. If you take the pressure off, then all of a sudden they want to survive. They're going to start making mutations. Some of those mutations will make them resistant to the antibiotic. They'll also start trading little bits of DNA that carry resistance genes. And those resistance genes have always been there - they're just not highly prevalent. So it's just a case of stopping them from sharing and concentrating those resistance genes into the bacteria that we have left that cause pathological infections.
Chris - What can we do about the problem?
Brad - Number one, I would say, is targeted treatment. You diagnose the bug and its susceptibilities before or soon after you start therapy. Number two is stewardship - you use the right antibiotic at the right dose for the right duration. Number three is prevention. There are things outside of antibiotics that we can do, like vaccination, hygiene, safe food, and safe water. Surveillance, number four, track what's happening locally. Because if you have an idea of what is already highly resistant or which antibiotics don't work in a local situation, you can change and perhaps treat them more appropriately. And then number five, I’d say, is something we call One Health. And that is outside of just human patients. You probably don’t realise that non-essential antibiotic use in agriculture and treating animals is equally driving bacterial resistance, because the bacteria are in the soil, it’s in the water, it’s in the environment. It’s not just going from one person to another. Some of this pressure isn’t just what we’re doing - it’s also what’s happening around us. Some places in these developing countries, you end up with issues where they’ve got poor sanitation. So a lot of times the bacteria will go through our digestive systems and end up in the sewers. But you’ve also got knock-off pharmaceutical companies that aren't getting rid of their intermediates appropriately. So that’s feeding into the same sewage. And all of this is happening at an ambient temperature of around 37 - 35°C - which is almost the perfect storm for these bacteria to mutate, to evolve, and to exchange these pieces of DNA. That’s where you end up with high concentrations of antibiotic resistance, and that’s why we see this in particular parts of the world. But like COVID, we know it isn’t going to stay there. All these resistant bacteria are going to move across borders. And the rate at which they move will largely depend on what we do here to try and make our antibiotics work better and longer.
Chris - Presumably there are also some practices - despite the fact that the risk exists in the environment and these microbes are out there - we can put in place to minimise the risk.
Brad - Definitely. Crowded wards help the germs spread. So we have to develop safe habits and make those habits the easy habits. For instance, things like putting hand gel at the end of every bed and near the door - use it on the way in, use it on the way out. Move patients as little as possible, because obviously it can spread from one patient to another. Keep people known to carry the same resistant germs together and away from others, or in single rooms - though that’s not always possible in low-resource settings. Dedicate the kit - thermometers, blood pressure cuffs, etc. - to those patients. But always things like clean water and working toilets. I suppose for the antibiotics we have, ideally you want to use quick, cheap tests to check if they're really needed. And then, probably after 48 hours, review that, and make sure that if they don’t need antibiotics, you don’t continue to use them. Or if it’s the wrong antibiotic, you change immediately to something that’s more effective. That way, you can sort of stop the process of concentrating these resistant bacteria and getting them to gain multiple resistances.

10:29 - Niger's AMR outbreak sheds light on where superbugs thrive
Niger's AMR outbreak sheds light on where superbugs thrive
Kirsty Sands, University of Oxford
Now, back to Kirsty Sands, whom we heard from earlier at the Ineos Oxford Institute for antimicrobial research. She has been looking at severely malnourished young children hospitalised in Niger and found that 3 in 4 of them were colonised with highly drug resistant bacteria, a situation which arose through significant spread between them in hospital…
Kirsty - We collected samples from just under 1,400 children. All of them were below the age of five. We collected rectal swabs as a less invasive tool for us to screen the gut microbiome. We were really interested in trying to understand what bacteria were colonising within the gut and inferring whether or not this could be a risk for ongoing infection and ongoing transfer to other children and into the environment. We began by culturing them to have a look at what was growing from these samples. To complement our work, we also used some genetic approaches, and some whole genome sequencing, to understand the genomic traits of different bacteria.
Chris - And was this just done once when the kids first came in, or did you look multiple times?
Kirsty - Multiple times. This was a study that progressed over time. We collected the first swabs when the patients were admitted and then we collected samples throughout their hospital stay for those children that were quite unwell, and then for everybody we also collected a swab at patient discharge. This gave us the ability to look at those different environments, so whether the bacteria were present at the beginning or whether they picked up particular drug-resistant bacteria during their stay.
Chris - When you give people antibiotics you can drive the development of resistance to those antibiotics - but also they could be picking up resistant bacteria from other kids who are in the environment. So I suppose there are two sources through which resistance could flow here?
Kirsty - Yes, absolutely there are. I think one of the most important aspects is to be able to understand whether the resistance is within the bacteria itself in terms of the core gene, or whether it's being carried on what we call plasmids, which are mobile, often circular structures that the bacteria can pick up and pass on in many different situations. And in our study, that’s what we found - the bacteria had these plasmids with antibiotic resistance genes.
Chris - So does that argue then that because these kids are being put on antibiotics, there is a risk that they’re going to acquire resistance from the environment they’re in? And did you find that was happening - that there was a spread of resistant forms around these children as they were hospitalised?
Kirsty - We did, in large numbers unfortunately. Some children were colonised with these drug-resistant bacteria at the beginning. However, over two-thirds of the patients that were negative for a particular drug-resistant E. coli on admission became colonised by the time we collected the sample at patient discharge. This suggests that within that environment and within that time frame, they are picking up this bacteria from somewhere. It’s quite a concerning finding in the fact that in a short space of time extremely vulnerable patients - who of course are admitted to a treatment facility for a very good reason - are leaving the treatment facility carrying a drug-resistant E. coli that may well go on to pose a threat to the wider community.
Chris - So what should we do about it? Do we know that they do actually pose a threat and they're going to carry on hanging on to those resistant forms, is there evidence of onward harm?
Kirsty - There is evidence of onward harm more widely. We have to think that these bacteria, you know, because they can persist in different environments, they can be found, different samples, different sources, there's always this possibility of an ongoing concern. I think, following this project, it would be really important to know whether the same bacteria we found colonising the children was found within the treatment facility. This would really drive the need for access to more suitable and sustainable infection prevention and control strategies. It would be essential to know how long these children remained colonised for and how long that potential threat exists in the community.
Chris - Right now, of course, we’ve got serious problems in the Middle East, and it almost looks like we’re going to have history repeating itself - based on what you found in Niger - in Gaza.
Kirsty - Yes, absolutely. We are seeing all the same problems. There's a huge shortage of food, which will increase the levels and numbers of malnutrition in children in particular. A large amount of overcrowding. It’s a very, very tough situation, which would then mean that there are limited resources and access to clean, safe drinking water. Hygiene and sanitation will be very difficult to maintain. What this really means is that we will see an increase in drug-resistant bacteria and we will see an increase in the spread of these bacteria across people, across the environment, and this may well be a broader threat to other countries.

17:06 - Cuts to UK Fleming Fund could cause global AMR blind spots
Cuts to UK Fleming Fund could cause global AMR blind spots
Jeremy Knox, Wellcome Trust
In 2015, the UK government set up the Fleming Fund, committing £250 million to fight antimicrobial resistance across Asia and Africa. It was an enlightened move because, as we keep saying, what goes around comes around, and so we need to keep an ear to the ground, microbiologically speaking. But, in July, the shock announcement came that funding would be withdrawn and the initiative would be closing down. This move echoes a worrying trend set by the US in cutting foreign aid spending. Jeremy Knox is head of policy for infectious diseases at the research charity The Wellcome Trust…
Jeremy - Turning off the funding, removing the funding that had been available through the Fleming Fund, is undoubtedly going to have a very significant impact in terms of their ability to actually do the type of monitoring, the type of disease surveillance they've been doing. In terms of how we quantify that impact, that's very hard to say, but clearly if the laboratory capacity that's been built, if the capabilities that have been developed using Fleming Fund money, is lost, then that really is going to impact those health systems and national governments, in terms of being able to understand the problem in their country, to make sure they're treating patients effectively, to make sure they're mounting an effective national response to AMR. The other element is the global element, and I guess there’s two sides of it. I think firstly, the Fleming Fund has been supporting a great deal of work, including some that Wellcome had co-funded.
When the fund was set up back in 2015, we didn't have a single estimate, or a credible estimate, of what the overall global burden of AMR looked like. The Fleming Fund has helped fund research which has given us a much better understanding now of what that global picture looks like, what the country-level estimates look like, and then what the trajectory is of the patterns of drug resistance. Then in terms of the wider global picture, as we lose that understanding and we lose the capabilities to deal with drug-resistant infections in poorer countries in Africa and Southeast Asia, like so many infectious disease problems, a problem anywhere can very quickly become a problem everywhere. Drug-resistant bacteria, like any infection, don't respect borders. So it was a very sound investment. It was a real win-win to be supporting efforts to improve surveillance, to improve the response to AMR in low- and middle-income countries, because that improves global health security and makes sure that we don't have problems of AMR developing and spreading around the world before we can effectively control them.
Chris - The Wellcome Trust is a pretty powerful entity, and you have the ear of some pretty
powerful other entities. Is this a void that you can step into, to try to offset some of those difficulties that you've just outlined?
Jeremy - AMR is not unique at the moment in terms of facing real funding challenges. Of course, we've seen in the last six months or so what's been going on with the US making significant funding cuts to its investments in all sorts of different areas, and that having a very profound impact. Of course, we - as a major global funder of AMR, but of other issues as well - we will try and address issues that arise because of this where we can, but we don't have the capacity to close the gap that's left by the US government or by the likes of the UK government.
Chris - Who actually killed off the Fleming Fund though? Because one journalist - from one of our major radio networks - phoned me up and asked me for my opinion on it. She said, this seems to have flown under the radar. People don't seem to have realised this is going on. And she wanted to make a particular thing of it on one of our flagship news radio programmes. So who is responsible for pulling the plug? And is this an irreversible decision? Can we not point out to them the error that is intrinsic to this decision and try to get it reversed?
Jeremy - It's hard to say exactly where the decision was taken. But I think clearly it's in the context of the UK government having to make, unfortunately, cuts to its overseas development spend. We're seeing a lot of reductions across the piece in global health that we're very concerned about. For instance, we're seeing significant cuts in the amount of R&D spending that comes from ODA - Official Development Assistance, to use its technical term.
In terms of a question of whether the Fleming Fund decision is reversible, that's hard to say. But what we have heard from ministers is that they are committing to working very hard to make sure that there isn't simply a loss of the capabilities, or the networks, and learning that have been built by the Fleming Fund over 10 years of excellent work. They have said they will think about how they can try to mainstream it within things that the FCDO - the Foreign, Commonwealth and Development Office - do, or by asking countries to build work on AMR into what they do on pandemic preparedness.
So I think we've heard the right noises in terms of making sure we don't have a total loss of what the fund has been doing. But I think we will need to keep a very close eye on that and make sure there is follow-through, and that AMR is still seen and championed as a priority. And, as I said, that AMR becomes more of a mainstream issue alongside other country-level health imperatives, and that the UK continues to support and champion that.

22:19 - What can science and policy do to tackle AMR?
What can science and policy do to tackle AMR?
Colin Brown, UKHSA
Tracking and tackling antibiotic resistance requires a joined-up global effort, and new scientific innovations to help us to stay one step ahead. Colin Brown is an infectious disease clinician at the UK Health Security Agency, and a leading expert on AMR. What does he think we need to be prioritising?
Colin - So I think there are multiple areas where science can help. Number one is new drugs. As the drugs we have cease to be effective, we need new drugs to replace them that are effective. And we in the UK have a scheme to try and incentivise drug companies - often referred to as the "Netflix model" - whereby we pay a subscription fee, as it were, for companies. Regardless of whether we watch something once or watch it a million times, or whether we use the drug once or use it a million times, we give them the same price point. That is because antibiotics have very - unfortunately - poor investment potential, because once we have a new antibiotic, we don’t want to use it widely - we want to restrict it for cases where it’s absolutely necessary.
And that is not a very attractive prospect if you're trying to develop a drug, whereas you could be investing money, for example, in a new anti-cancer drug, or a new heart drug, or a new weight loss drug that you might be able to give to lots and lots and lots of different people, as much as possible. We also really need to understand best where resistance is developing and where it’s being transmitted. We know that as people get exposed to antibiotics, resistance will develop, but that happens also in the environment. It happens in animals that we eat or interact with.
And trying to ascertain where do you get the best bang for buck in prevention efforts? Is it about screening people so that you pick up drug resistance early in healthcare settings, and you prevent it transmitting from one patient to another patient to another patient? Is it about better drug awareness and people only taking if they definitely need them as prescribed, and perhaps investing more in diagnostic tools that really help us to find where the best use of antibiotics is only in those people that really need them? So there’s a variety of different things that we need to do. Some artificial intelligence will definitely help us with; a lot of modelling and looking at where of all the different interventions we could do, we will get that best bang for buck. And some of it is about what's coming down the line and how do we invest in new antimicrobials so we have new antibiotics when we need them?
Chris - This is arguably a big problem in hospitals. Once you get people into hospital, because of the close contact - just as we were hearing earlier in the programme in Niger - when kids come into hospital, close contact means they’re more likely to acquire these things. So are we also looking at the behaviours of hospitals, how we manage patients, how we manage staff, to minimise the opportunity for these bugs to spread among patients and staff?
Colin - Most definitely. Infection prevention and control efforts in hospitals are key to preventing that spread. People have large amounts of bacteria that have been exposed to very broad-spectrum antibiotics that are sort of blunderbusses that treat all manner of both infections and normal bacteria. There’s lots of patients who are very unwell, who don’t have control over their bowel movements. There's lots of potential routes whereby there's both the resistant antibiotics and the means of them spreading around.
In places like Niger, it’s all the more difficult because they also don't have the water and sanitation and hygiene practices we often take for granted in the UK. One big aspect is helping hospitals with their infection prevention and control, and some of that is modelling work and identifying what is it about practice that is likely to interrupt the spread? Is it screening people and isolating them if they carry resistant bacteria? Is it hand hygiene - which we know throughout the world we could improve on? Is it around patients meeting each other in different areas of the wards and interacting and spreading bacteria that way? Is it the cleaning of toilets, showers, and washrooms? For example, we're trying to look at: can we do with waterless toilets and waterless sinks to try and prevent splash of bacteria that may transmit from person to person? So at every stage of that, there is a range of different science advances.
Chris - This is arguably a global problem, and global problems need global solutions. Is everybody everywhere on the same page with this, or do we have a fragmented landscape? No joined-up thinking and therefore - because the weakest link in the chain is always the place it's going to break - as soon as one bit breaks down, we’ve got a problem and it’s a problem everywhere.
Colin - I think everyone is broadly on the same page for what we want to do. There clearly is a difference in resources. The UK has provided significant assistance to many countries and continues to do so through things like GAMRIF - the Global Antimicrobial Resistance Innovation Fund. We work closely with countries as part of the UK Health Security Agency, particularly in Nigeria, Ethiopia, and Zambia, do a range of development work, which does include antimicrobial resistance. And we do the same also in the Caribbean with some of our UK overseas territories. There are lots of countries that want to be doing really good work here, but they have multiple challenges facing their health systems, of which AMR is only one.
And there are some basics that are difficult to access, for example, clean water. They also have less in the way of access to novel drug agents to be able to help where there are resistant bacteria to treat. So there are a wide number of problems that parts of the world face. So in that way, it is a global effort. A lot of the work that we are doing as an organisation has direct relevance to any setting.
So, where best to invest your money? How do you best prevent transmission of resistance once it develops, and prevent the development of resistances either in people, animals, or the environment? All of that has got real global applicability once we identify some of the key learning. So in that way, the work that we are doing really is trying to help the globe. But we do need to recognise this is an interconnected problem, and that if a part of the world that we see regular travel from or regular healthcare from has got a problem, then all too soon we will have a problem. That fits in with some of the screening recommendations that we recommend nationally, whereby if we know people are coming from areas where there is more antimicrobial resistance, we do recommend that particularly if they've been exposed to healthcare environments there, they get screened.










Comments
Add a comment