This week's Pathological programme brings you a glimpse into the world of the pathologist. We attend a real autopsy to discover how a pathologist uncovers a cause of death, and hear how Cambridge scientists have found a new way to stop Multiple Sclerosis (M.S.) in it's tracks. We also find out how a common rock can lock away carbon, why forest fungi give out less greenhouse gases when they're warm, and shed some light on the workings of world's smallest solar panels. Plus, in place of Kitchen Science, Ben tries to stop a virtual outbreak of the plague!
In this episode

Rock-steady way to tackle rising Carbon Dioxide
Barrack Obama has famously pledged to put the US at the forefront of global warming (cynics would say it already is!), so it's fitting that a US scientist has this week developed a strategy that could lock away literally billions of tonnes of CO2 per year.
 Writing in this week's PNAS, Columbia University geologist Peter Keleman explains how it should be possible to use the same mechanism that has controlled CO2 levels on Earth for billions of years to cut greenhouse gases today.
Writing in this week's PNAS, Columbia University geologist Peter Keleman explains how it should be possible to use the same mechanism that has controlled CO2 levels on Earth for billions of years to cut greenhouse gases today.
His approach revolves around one of the most abundant minerals on the planet called olivine, which is a form of magnesium silicate. At the Earth's surface this chemical readily reacts with carbon dioxide and water to form magnesium carbonate (called magnesite) and quartz (silica), thus locking the CO2 away as rock. Keleman has shown that CO2 warmed to about 30 degrees Celsius and pumped into seams of olivine rapidly kickstarts the chemical reaction, which itself produces heat, accelerating the process further.
"Our data suggests that about 4 billion tonnes of CO2 per cubic kilometre of rock involved in the process could be locked away with this process," Keleman explains, "and given that we currently produce about 30 billions tonnes per year, and Richard Branson has offered a substantial cash prize to anyone who can lock away 1 billion tonnes of CO2, we're definitely in the right ball park."
The good news is that wherever there are mountains there are rich deposits of olivine, and some countries are extremely well endowed with the mineral including the Balkans, Saudi Arabia, the United Arab Emirates and Papua New Guinea. So is Keleman suggesting we need to ship our waste CO2 to these places? Not quite; in this instance Mohammed will have to come to the mountain.
"I think in the future we'll see a migration of CO2-producing industries and electricity-generating facilities to areas with the capacity to lock away CO2 using technqies like this."

A fungal solution to climate change?
The fight against future climate change may have an unexpected ally, in the form of mushrooms living on the soils of northern Spruce forests of Alaska, Canada and Scandinavia.
 Steven Allison and Kathleen Tresede from the University of California Irvine conducted experiments in Alaska and found that when temperature increases, fungi living on the forest floor dry out and emit less carbon dioxide, the opposite of what the researchers expected to find since colder climates are thought to slow down the processes by which fungi produce carbon dioxide.
Steven Allison and Kathleen Tresede from the University of California Irvine conducted experiments in Alaska and found that when temperature increases, fungi living on the forest floor dry out and emit less carbon dioxide, the opposite of what the researchers expected to find since colder climates are thought to slow down the processes by which fungi produce carbon dioxide.
The study, published in the journal Global Change Biology this week, involved Allison and Tresede going out into the forests of Alaska and setting up several small greenhouses. At the start of the experiment - the beginning of the growing season in May - the scientists kept the conditions inside the greenhouses the same as in nearby control plots. Then, they closed the greenhouses and the temperature of the air went up by 5 degrees Celsius, while the temperature in the soil went up by 1 degree.
By carefully measuring the gases in all these experimental plots they found that by the end of the growing season in August, the amount of carbon dioxide produced by the soil in the greenhouse plots was around half of that produced in the unheated control plots.
Allison and Tresede found that there was about half as much fungi inside the heated greenhouses as in the unheated plots, indicating that when the temperature increases, much of the fungi die while some become inactive and stop producing as much carbon dioxide.
What we don't currently know is whether this change in carbon production will have a significant effect on the climate. Halving of the CO2 output with a 5 degrees increase in temperature certainly sounds like a major change. And this could be particularly important since northern forests are thought to lock away half of the world's soil carbon.
But of course we know very little about how the ecosystem as a whole might respond and adapt to increasing temperature over the longer term and what other changes might be triggered. Ecosystems are notoriously complex, unpredictable things.
There is also the possibility of knock-on effects of this reduction in fungal activity. The soil fungi are doing a really important job of breaking down dead organic matter like fallen leaves, so presumably, halving their numbers could well have an important effect on the functioning of the ecosystem.
While these findings certainly help us understand a little better what is going on and for once this is something that could help alleviate the problems of climate change rather than make them worse, but the picture is still not clear cut and this certainly won't mean the end of global warming.

Booze-prone brain behaviour
Scientists have uncovered a genetic reason why some people are prone to alcoholism.
 University of Massachusetts Medical School researcher Gilles Martin and his colleagues, writing in this week's PNAS, have found that one of the components of a pore (called the BK channel) found on the surfaces of brain cells can predispose to the rapid development of alcohol tolerance. This pore allows potassium to enter nerve cells, helping to damp down nerve excitability. But alcohol makes the pore remain open for longer than normal, reducing nerve activity and thus accounting for its depressant effects.
University of Massachusetts Medical School researcher Gilles Martin and his colleagues, writing in this week's PNAS, have found that one of the components of a pore (called the BK channel) found on the surfaces of brain cells can predispose to the rapid development of alcohol tolerance. This pore allows potassium to enter nerve cells, helping to damp down nerve excitability. But alcohol makes the pore remain open for longer than normal, reducing nerve activity and thus accounting for its depressant effects.
But in some people, despite the continued presence of alcohol, the channel quickly returns to its normal activity, which could urge the drinker to consume even more alcohol to maintain the intoxicating effect. Individuals who show this kind of nerve cell behaviour seem to be more prone to alcohol dependence, although scientists had no idea how it happens.
To find out Martin and his team first knocked out a gene called beta4, which codes for part of the BK channel targeted by alcohol. Tests on nerve cells in these animals showed that, compared with normal mice, the cells very quickly returned to normal after alcohol exposure. Putting the beta4 subunit back, on the other hand, made the channels recover much more slowly. So perhaps, suggests Martin, that individuals with a tendency to alcoholism might have mutations in their beta4 genes which affects the levels of the protein in their brains, or how it controls the BK channel activity in the presence of alcohol.
"This we need to find out," he says. "And then perhaps this will lead to tests that can enable doctors to spot people at risk of alcoholism, or perhaps the development of novel drugs to compensate for the altered channel activity which might reduce a person's risk."
The world’s smallest solar panels
The world's most minute solar panel cells have been built and tested and one day in the not too distant future they could be used to power even tinier microscopic machines.
![]() The solar panels were built by Xiaomei Jiang and her team of researchers from the University of South Florida in the States.
The solar panels were built by Xiaomei Jiang and her team of researchers from the University of South Florida in the States.
Their study published in the Journal of Renewable and Sustainable Energy describes how they built tiny solar panels about the size of a lower case o in 12 point font on a computer.
To make these tiny solar cells the researchers didn't simply take normal photovoltaic solar panels - the kind you might see on rooftops - and make them much smaller.
Regular solar panels are built on a brittle backing material made of silicon, similar to the sort of thing computer chips are built on. Instead, these tiny solar cells are based on an organic polymer that has the same properties as silicon, but that can be dissolved into a fluid and printed into a flexible backing material. Theoretically, this organic material could be sprayed on any surface that is exposed to sunlight.
Jiang and her team are developing these tiny panels with the hope that they will one day power a type of microscopic sensor that can be used for detecting dangerous chemicals and toxins.
These detectors are built from carbon nanotubes, the tiny cylinders of carbon that are 50 thousand times thinner than a human hair. The idea is that when the nanotubes are hooked up to a power source of around 15 volts, they can detect small amounts of particular chemicals by measuring the electrical changes that occur when chemicals enter the tubes; the exact change in charge is an indicator of what type of chemical is present.
So far, the team have put together an inch-long array of 20 of these tiny solar cells which has been enough to generate just 7.8 volts. The next step will be to optimize the cells so they produce enough power for the microscopic chemical detectors, which they think they will be able to do in the next generation of solar cells that should be ready by the end of the year.

14:31 - Kitchen Science - Plague Outbreak!
Kitchen Science - Plague Outbreak!
with Royal College of Pathologists and the Natural History Museum
Ben - For this week's kitchen science I have come along to the Royal College of Pathologists in London to join a team from the Natural History Museum to tackle an outbreak of infectious disease. Not a real one, you'll be pleased to hear, but an opportunity to see the real-life techniques used in this sort of situation. The first we heard about the outbreak was on the news.
News Anchor - We're here in central London at the site of what maybe the origin of a serious disease that has so far left several workmen critically ill in hospital and claimed the life of another. Building has disturbed a previously unknown medieval vault. Four days ago workmen unearthed this vault during routine excavation as part of the central London regeneration programme. Those involved are now critically ill in the London hospital of infectious diseases with one fatality already reported.
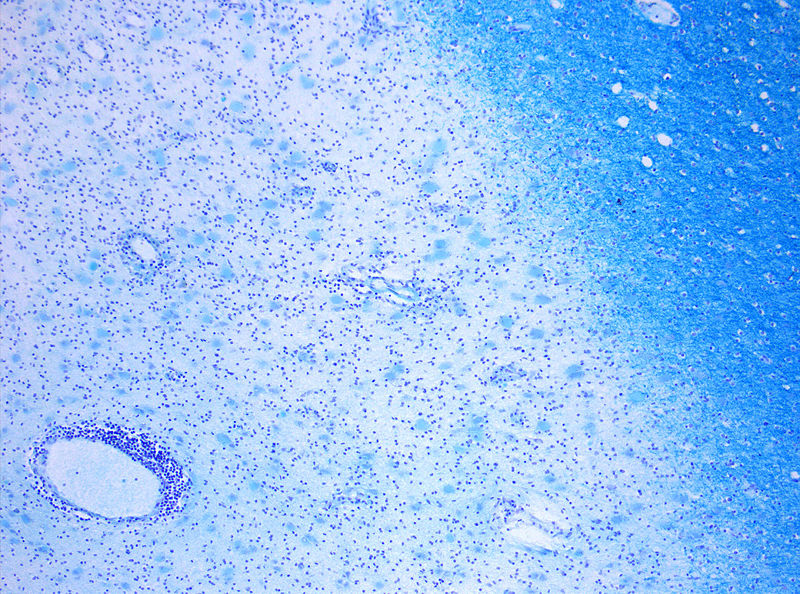
Ben - The workmen had stumbled across an ancient vault but it had a much more recent corpse inside. To find out what had happened to the corpse in the vault and give us clues as to what could be wrong with the workmen Dr Nicky Cohen took me through the results of an autopsy.
Nicky - So we have a body in front of us and looking at him we can see that he's got some blood around his mouth and his eyes. He's got blackened toes and fingers. That blood picture is making me thing he's got a blood clotting disorder. On top of that he's got some insect bites around his ankles. He's got a swelling on the side of his neck. I don't know what it is, I'll take a sample of it later. Putting that together with the insect bites and the rats that we know were in the crypt I'm concerned that he's got an infection and he's died of an infection which would fit with the live bodies. The patients in the hospital. As to what causes this I think it's difficult and I don't know but I guess something like mumps is an infection that can produce swollen glands in your neck but not many people die of mumps, of course. We know there were rats involved so leptospirosis, Weil's disease might give us something similar to that and that can cause blood clotting disorders. In terms of putting that altogether with the lumps in the neck what I'm most concerned about is Yersinia pestis which is plague and we need to do some tests to find out what it is.
 Ben - by looking at the sample taken from the swelling in the neck under a microscope we were able to confirm the worst. The swelling contained Yersinia pestis bacteria, the plague. There are two stages of plague infection: bubonic and pneumonic. Bubonic plague causes the distinctive swellings on the body or buboes but is transmitted from one person to another through a vector, in this case, fleas. Most people think of plague as a medieval disease, long-since wiped out. But Martin Hall, and etymologist at the Natural History Museum explains how outbreaks of plague still happen today.
Ben - by looking at the sample taken from the swelling in the neck under a microscope we were able to confirm the worst. The swelling contained Yersinia pestis bacteria, the plague. There are two stages of plague infection: bubonic and pneumonic. Bubonic plague causes the distinctive swellings on the body or buboes but is transmitted from one person to another through a vector, in this case, fleas. Most people think of plague as a medieval disease, long-since wiped out. But Martin Hall, and etymologist at the Natural History Museum explains how outbreaks of plague still happen today.
Martin - Plague is found naturally in rodents in places like South East Asia, South America, Africa. There are wild rodents that have plague naturally in them. They actually don't really suffer. They don't die from the disease. They're acting as what we call, reservoir hosts. They just maintain the disease. Now and again something happens to break that cycle. There might be a big outbreak of rates and those rats become infested with the plague and these domestic rats are much more susceptible to plague and they can die. When they die the fleas that were feeding on them don't have anything to feed on so they go looking for something else to eat. They may land on you and bite. Then the bubonic plague is transmitted to you. It seems that the corpse in the vault contracted the plague and then died in the vault. The fleas living on the rats in the vault picked up the bacteria and passed it on to the workmen when they discovered the vault. Bubonic plague is treatable with antibiotics but if this outbreak continues the plague could progress to become the pneumonic form which is spread through the air and has a 90% fatality rate. The clock is ticking for us to take control of the outbreak before this happens. This is where I need your help. What should we do to contain the outbreak and avoid a national epidemic of plague? I asked a few other amateur pathologists who had come along for the event.
"We'll kill every rat we see""You need to let all of the police know in the area so they can notify those who are in charge of communicable diseases"
"We said to trap the rats and then poison them. But then you're saying about the fleas - maybe burn the rats and that will get rid of the fleas. Then we can quarantine anyone that has symptoms."
Ben - So what steps do you think we should take to quarantine an outbreak of plague? Can all the rats shut down the underground? Quarantine central London perhaps?
Ben - So far we've been faced with the very real possibility of an outbreak of plague in London and asked what would be the best things to do to try and contain it. At the Royal College of Pathologists we decided to kill as many rats as possible and use pesticides to control the fleas, quarantine the affected and call the Health Protection Agency. Dr Tim Wreghitt who is from the HPA and Addenbrooke's hospital explained what he thought of our containment techniques starting with killing of the rats.
 Tim - The idea is that you can't control rats and you can't get rid of fleas but the more you reduce the population the lower you make the risk. You can't eliminate them you try everything you can to reduce the number in a particular area. Quarantine the infected area, that's really important. You need to know where the new cases are. This is where this is a really good thing - tell health professionals. I think that's one of the most important things you've got round here. This is a very rare disease, very few medical people in this country will have seen a case of plague because it doesn't occur in this country. You've only got the odd case that may come in as an imported disease. Most people couldn't recognise it if it was their neighbour and so they need to be told what the symptoms are. You need extensive health programme to educate health professionals and to alert the Health Protection unit about these cases. Then you can find, those cases, isolate them and something you haven't mentioned is giving antibiotics because this is a disease which is controlled by antibiotics if you give it within 24hrs after people get symptoms. Finding the people really quickly with the relevant symptoms, giving them early treatment with cibrofloxacin or something like that will make the mortality go down from 60% to less than five percent. It's really important. Also those people who have been exposed to cases, if you give them prophylactic antibiotics by which I mean as soon as they've been exposed to the risk you then give them antibiotics to prevent them getting the infection. That's really important as well.
Tim - The idea is that you can't control rats and you can't get rid of fleas but the more you reduce the population the lower you make the risk. You can't eliminate them you try everything you can to reduce the number in a particular area. Quarantine the infected area, that's really important. You need to know where the new cases are. This is where this is a really good thing - tell health professionals. I think that's one of the most important things you've got round here. This is a very rare disease, very few medical people in this country will have seen a case of plague because it doesn't occur in this country. You've only got the odd case that may come in as an imported disease. Most people couldn't recognise it if it was their neighbour and so they need to be told what the symptoms are. You need extensive health programme to educate health professionals and to alert the Health Protection unit about these cases. Then you can find, those cases, isolate them and something you haven't mentioned is giving antibiotics because this is a disease which is controlled by antibiotics if you give it within 24hrs after people get symptoms. Finding the people really quickly with the relevant symptoms, giving them early treatment with cibrofloxacin or something like that will make the mortality go down from 60% to less than five percent. It's really important. Also those people who have been exposed to cases, if you give them prophylactic antibiotics by which I mean as soon as they've been exposed to the risk you then give them antibiotics to prevent them getting the infection. That's really important as well.
Ben - So we were right to quarantine the area, call in the experts and start trying to control the vector but because we didn't think of prophylactic antibiotics the mortality rate would have been higher than it should be. The real question is did we do enough to contain the outbreak? To find out we have to go back to the news.
News Anchor - We return now once more to the scene where several weeks ago, we reported on the mysterious illness that had affected several workmen and tragically claimed the life of another. We're joined by Amy Stevens from the Health Protection Agency. Amy, can you tell us a bit more about the strategy and measures you used to stop this disease in its tracks?
Amy - Following extensive analysis we were able to identify that the bacteria was Yersinia pestis, better known as the plague. Thankfully today this is a disease that is easily and effectively treated with antibiotics. Infected individuals from the area and from the worksites were quarantined and treated and were kept under constant surveillance until it was shown they were clear of infection. It is now completely absent from the site. We consider it to be successfully contained.
News Anchor - That's great news. Thank you, Amy
Ben - So the measures we put into place were enough to contain the disease and avoid a major outbreak. If you thought of the same sorts of things well done! You're the kind of person we need around if there's ever an outbreak of plague.
20:26 - Multiple Sclerosis: Successful Treatment
Multiple Sclerosis: Successful Treatment
with Alistair Coles, University of Cambridge
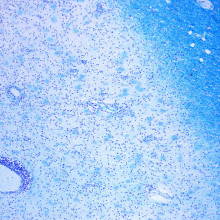
Alistair - If you see a young adult in this country that is disabled then the likely thing is that they have multiple sclerosis. This is the commonest disease of the brain and the spinal cord amongst Caucasian people in the west. It's a disease where the immune system attacks a particular part of the nerve in the brain or in the spinal cord. That particular part is the myelin sheath. What that means is the insulation that covers the nerve. This means that nerves can lie across each other and short circuit or impulses intended for one area can cross over to another nerve and not reach their target. You get electrical confusion in the brain.
Chris - Does this happen everywhere or is it quite discrete bits in the brain that get affected?
 Alistair - You're quite right. The immune attack is just on specific patches within the brain. Each patch will go through a period where there is lots of inflammation. It may cause symptoms but then it resolves and dies away to leave some scarring only for other areas of the brain to become involved.
Alistair - You're quite right. The immune attack is just on specific patches within the brain. Each patch will go through a period where there is lots of inflammation. It may cause symptoms but then it resolves and dies away to leave some scarring only for other areas of the brain to become involved.
Chris - Do you know what bits of the immune system are doing that damage?
Alistair - Multiple Sclerosis is one of these diseases where we are all capable of getting it. If I looked in your blood, or in my blood or anyone else's blood we would find cells of the immune system: T-lymphocytes that are aggressive towards myelin, towards the brain. The thing that's stopping you or I from getting Multiple Sclerosis is that we have another set of cells called the regulatory T-cells which prevent the aggressive T-cells from carrying out their attack. In people who have Multiple Sclerosis the defect is that their regulatory T-cells are not working properly.
Chris - So what have you been looking at in terms of how to get people to have the best outcome possible for them?
 Alistair - Our initial logic was very simple. It is to say MS is a disease where the immune system attacks the brain. Let's disable the immune system and it will no longer attack the brain. We looked around for a drug that might do that and we came across alemtuzumab, or as it was known then CamPath. We said that this is a drug that deliberately hones in, identifies and kills one of the cells of the immune system: the lymphocyte. It disables the immune system very effectively.
Alistair - Our initial logic was very simple. It is to say MS is a disease where the immune system attacks the brain. Let's disable the immune system and it will no longer attack the brain. We looked around for a drug that might do that and we came across alemtuzumab, or as it was known then CamPath. We said that this is a drug that deliberately hones in, identifies and kills one of the cells of the immune system: the lymphocyte. It disables the immune system very effectively.
Chirs - What was the nature of that trial? How many people were there and what did you do?
Alistair - This is a trial that we have recently announced the results of. It consists of 300 patients studied over 3 years. We are comparing the new drug against the standard licensed therapy of MS, which is beta inteferon. This is a head to head study saying "does this new drug alemtuzumab work better than beta interferon"? The results were that alemtuzumab is vastly more effective than beta interferon. It does three things, firstly it reduces the chance of having an attack of MS over three years by over 70% compared to taking the standard treatment. Secondly it reduces the chance of becoming disabled over three years by 70%. Both of those things we were expecting. The third result, which we weren't expecting, is that at the end of three years patients who had taken alemtuzumab or CamPath were actually less disabled than they had been at the start of the study. So three years later they were now more able to work, more able to look after their families and more able to play their sports. That has forced us to go back and ask whether we really understand the disease of MS. Up until now people have always thought that once you have got disability from MS that is due to permanent scarring in the brain and that will never get better. We had imagined that the best we could get out of any treatment of MS is that people would just stay the same and not get any worse. Amazingly we now see people getting better.
Chris - What do you think is going on?
Alistair - We are back to the drawing board on this. One idea is that when the immune system recovers after being attacked by this drug, alemtuzumab or CamPath, immune cells grow back which are capable of getting into the brain and secreting factors that promote repair and survival of neurons and of the cells that produce myelin oligodendrocyte. That's certainly not what we were expecting but we found it to be true.

26:13 - The Royal College of Pathologists
The Royal College of Pathologists
with Adrian Newland
Helen - Professor Adrian Newland is the president of the Royal College of Pathologists. We are honoured to have him with us in the studio right now. Hi, Adrian. Thanks for coming in. It's great to have you with us. We thought we would start off by asking you what does it constitute to be a pathologist? Who are pathologists?
 Adrian - The simple answer to that is pathologists are involved with diagnosis. There are at least 18 different types of pathologists involved with all aspects of the living from pregnancy and infertility right through to death and fatal diseases. Many of those types of pathologist look after patients and are involved in their care on the wards in addition to diagnoses. Many are also involved in the research behind the diseases. We are very keen to look at the basis of disease. We are involved in research and development to try and find out why diseases happen and how we can improve treatments.
Adrian - The simple answer to that is pathologists are involved with diagnosis. There are at least 18 different types of pathologists involved with all aspects of the living from pregnancy and infertility right through to death and fatal diseases. Many of those types of pathologist look after patients and are involved in their care on the wards in addition to diagnoses. Many are also involved in the research behind the diseases. We are very keen to look at the basis of disease. We are involved in research and development to try and find out why diseases happen and how we can improve treatments.
Helen - So it's really everything about diseases I guess. Is it just doctors that are pathologists?
Adrian - No, there are a group of scientists as well. 20% of the members of our college are actually clinical scientists. We work together as a team in all aspects of diagnosis, research and patient care.
Helen - You are a haematologist, is that right?
Adrian - Yes that is right.
Helen - So you deal with blood. I gather you talk to and meet patients as well as working on the research side. You must have an insight already into how diverse a job being a pathologist is.
Adrian - Yes I cover all those aspects. In fact it was one of the big attractions of going into the specialty. The fact that I could look after patients and take their blood, then take it to the laboratory and be involved in the diagnosis. I didn't have to send a sample off then get a result back on a bit of paper and deal with it. That is the whole exciting element of that as an area to work in.
Helen - You are President of the Royal College of Pathologists. What exactly is the role of that organisation? What do you do?
Adrian - We have 4 main aims. We are involved in training, particularly training trainees in pathology. We are involved in maintaining standards and developing guidelines. We are involved in promoting research. We are also involved in educating the patients and public in what pathology is and what their diseases are and to give them an awareness of their bodies.
Helen - This week is national pathology week. This is the first time this has ever happened. What was the idea behind having this week?
Adrian - We've been doing some work at the college in developing an education centre and that was finished this month. We took it over and we thought we would celebrate this by actually developing the part of our mission which was patient awareness and patient education. A national pathology week seemed a great way of doing that. The enthusiasm we've had from members of the college around the country has been absolutely fantastic.
Helen - I would have thought, maybe on the surface, that things on TV like CSI and all those programs dealing with autopsies and the forensic side of things would be good in creating awareness of pathology? You think it maybe is not such a good thing?
Adrian - I don't think it is. I think that is fine and we want to put the forensics into perspective. Many patients and the public are not even aware we are doctors. So I think it gives a rather distorted idea of what pathology is.
How are blood cells made?
We put this to Professor Adrian Newland:
Adrian - Blood cells are made in the bone marrow. In the bone space - in particular in the pelvis, in the bones of the back, the ribs and the sternum. They're made from stem cells that then incorporate protein, iron, all the building blocks of haemoglobin that then encapsulate in cells that are pushed out into the blood. Many millions of cells every day.
What role do the appendix and tonsils play?
We put this to Professor Adrian Newland:
Adrian - The gut has lots of areas of immune system throughout it to try and deal with any infections that come in through the mouth and go down into the gut. The tonsils themselves are particularly important early on in life. That is one of the reason kids and teenagers have such problems with their tonsils. They get exposed to airborne bugs. They stimulate the tonsils to develop immunities to those bugs and the tonsils get bigger and cause bouts of tonsillitis. Helen - I had my tonsils out when I was little and it wasn't very nice at all. Since then I've been absolutely fine.
Does the UK have a 'body farm'?
We put this to Professor Adrian Newland:
Adrian - Yes. I'm not aware of any body farms in the UK unless they are hidden away somewhere.
Chris - You're not aware of any body farms in America?
Adrian - No I'm not aware of body farms in America actually. We do have a lot of tissue banks that certainly have been regulated following the human tissue act that came through. These are a very important resource if researchers want to have material to look at, either disease or to look at normal tissue. If you want to find out the cause of a particular sort of thyroid for instance, you can get them from the bank. You can get 30 samples and look at them.

33:43 - The Process of a Post Mortem
The Process of a Post Mortem
with Alison Cluroe
Chris - Consultant pathologist Alison Cluroe took me through a case that she dealt with recently. Now the descriptions in this piece are quite graphic so if you are at all queasy or if you think you might be distressed by hearing how a post-mortem is carried out then you might want to turn off your radio for about ten minutes, which is roughly how long this took.
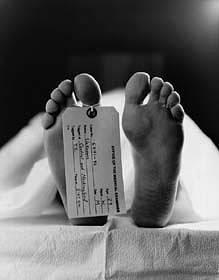 Alison - My name is Dr Alison Cluroe and I'm a pathologist. This morning I'm going to take you through a post mortem examination on a 72 year old lady who died at home. She had a history of high blood pressure, gout and indigestion. Of late she had complained of an abdominal distension. She went to see her GP but was very reluctant to go to hospital. The GP had arranged for her to undergo some tests and those were going to happen over the course of the next few days when unfortunately she died unexpectedly and suddenly at home.
Alison - My name is Dr Alison Cluroe and I'm a pathologist. This morning I'm going to take you through a post mortem examination on a 72 year old lady who died at home. She had a history of high blood pressure, gout and indigestion. Of late she had complained of an abdominal distension. She went to see her GP but was very reluctant to go to hospital. The GP had arranged for her to undergo some tests and those were going to happen over the course of the next few days when unfortunately she died unexpectedly and suddenly at home.
Chris - Presumably because we don't know why she died, the GP couldn't say, therefore it comes to you to try and work out what was going on with this lady and why she unfortunately died.
Alison - Yes, because the GP cannot issue a death certificate the case becomes a coronial case, referred to the coroner. He then looks at all the information and makes a decision as to whether we proceed to a post mortem examination to establish as to whether this is a natural death.
Chris - Looking at this lady what jumps out at you in your external examination. What do you think is going on here?
Alison - In essence she has a massively distended abdomen which does raise questions that some abdominal catastrophe has taken place. Looking at that distended abdomen I would be wondering has she got an intestinal obstruction? She certainly has evidence that she has been vomiting. That is clear from looking at the body. One would have to conclude that the likelihood that this is an obstruction. Whether it is an obstruction from something like an internal hernia, twisted bowel or tumour, we will have to wait until we do the internal examination.
Chris - The fact that she had a history of high blood pressure. Could that be an aneurism?
Alison - Yes. She does have a history of hypertension. One of the pathologies that goes hand in hand with that is an aneurism of the abdominal aorta. The aorta is a large artery running through the abdomen and on occasion in people with hypertension it can balloon out. The wall becomes paper thin, it's carrying a large amount of blood under pressure so there is a possibility that this balloon can burst with massive intra abdominal haemorrhage. So that would be another possible in the differential diagnosis.
Chris - The next step presumably is to open the body up and have a look at what is going on inside?
Alison - Indeed. At that point we undertake an evisceration which is done in combination with a mortuary technician. So now we are opening the chest and abdomen and we can see the distended abdomen very tight as the abdomen is opened. There is a large amount of blood stained fluid pouring from the opening and large loops of distended bowel packing the abdominal cavity. There is a small hernia next to the umbilicus, the belly button, where a small piece of bowel has pushed through the abdominal wall. It's a possibility at this moment that that hernia has caused an obstruction to the bowel and is responsible for a lot of the pathology that we are seeing here.
Chris - How would that happen if that were the case?
Alison - The small piece of bowel gets trapped within the hernial sac and obstructed so no fluid or food could pass further along the bowel. As more fluid is drunk and more food is eaten the bowel distends and distends and distends. This cause the abdominal distension that we see. As I'm watching this happening and I see the technician is starting to dissect a little bit further there appears to be some sort of tumour in here. So I'm beginning to change my thought processes as we go along here.
Chris - There's some little patches of it on the wall of the abdomen that we can see.
Alison - Yes, we can see here on the shiny peritoneal surface the lining of the abdomen there are several nodules of white tumour that are now apparent as we fold back the abdominal wall. It's also apparent that we've got large masses of tumour glueing the bits of small bowel and large bowel at the back of the stomach. It looks to me in fact that this lady has got a massive intra-abdominal tumour that's probably arising from one of the intra-abdominal organs.
Chris - Maybe bowel or maybe ovary?
Alison - Maybe bowel although with that pattern of spread I would be wondering about ovary. Commonly, bowel likes to go to the liver whereas ovary likes to go around the abdominal cavity. The pattern I'm seeing at the moment would make me think it's going to be an ovarian tumour.
Chris - I suppose if we now look through the organs that have been removed we might get some clues?
Alison - Yes, I think so. I think we should move on and have a look at the organs now. What I'm going to do is capture each of the organs individually. Starting with the spleen, it's a slightly softened spleen which suggests some underlying infection, not surprisingly with the degree of disease going on in the abdomen here in the intestinal obstruction. It doesn't appear to have any tumour in it. Moving on to have a look at the kidney I can see no evidence of tumour. There is, however evidence of surface scarring in this kidney.
Chris - It's not smooth, is it? There are some little pock marks on the surface. What are they?
Alison - That's right. The pock-marked areas would suggest previous episodes of kidney infection and pyelonephritis. These leave quite coarse scars on the surface. In addition, there's a very fine, granular scarring over the surface of the kidney which is something you see in people who have a history of hypertension: high blood pressure.
Chris - But that wouldn't have caused the present problem?
Alison - No. Those were incidental findings. If we move on to have a look at the liver - as I slice through the liver we can see two tiny tumour deposits which are the white, soft, fleshy tumours exactly the same as we're seeing within the abdomen.
Chris - They stand out really prominently, don't they? The liver's a nice, brown, very homogenous, regular colour in appearance. There are these white blobs standing there as if someone's actually pressed them on.
Alison - That's right. Very clear, well-defined nodules which are metastatic deposits of tumour. Thsi tumour has spread to the lady's liver.
Chris - Would it get there though the blood supply then?
Alison - Likely to be spread by bloodstream. Tumour's spread by three methods: direct spread, through the blood stream and through the lymphatic channels in the lymph nodes. In this case this would be blood-borne spread, yes. If we move on now to have a look at the thoracic organs, the organs within the chest and start by having a look at this lady's heart because we know she has a history of high blood pressure. That tends to make the heart enlarge. As we're examining it here I think you can see she does, in fact, have a big heart; a very meaty looking left ventricle of the heart. This is the one that pumps the blood around the body. It's quite evident that there is a thickening of the wall which would be compatible with the history as we know of high blood pressure. Looking at her coronary arteries these are the blood vessels that supply the heart. Often these become hardened with fatty deposits. In this case, in fact her coronary arteries are in very good condition. She has hardly any atheroma.
Chris - Yes, I wish my heart was that good. I suspect it's not but, this looks less normal here. What's this?
Alison - Yes, as we're moving on now actually looking at this lady's trachea - her main airway from the back of her throat. That airway is packed with vomit so she has aspirated vomit. If we now move on to look at the lungs you will see that all the tiny airways extending all the way out to the periphery of the lung are packed with this vomit. Unfortunately the actual final cause of death in this lady is her massive aspiration of gastric contents.
Chris - And that would have cause asphyxia, presumably?
Alison - Yes, essentially she would have asphyxiated and been unable to breathe as a consequence of that. We need to actually now go to the main source of the problem which will explain why she has had such a massive aspiration of vomit. We have here the gastro-intestinal system and we can see that the small bowel is massively dilated. As we move down its length there's a huge, huge lump of tumour that completely encloses and encases the bowel and has essentially obstructed the bowel.
Chris - Does this give you any clues as to what sort of tumour this is yet, though?
Alison - Well, I think I'm still of the opinion that I would say there's been an ovarian primary tumour. We've opened the bowel, we're looking at the bowel from the inside. I can't see any tumour arising from within the lining of the bowel which is where you would expect a primary bowel cancer to come from.
Chris - I guess the answer is to actually take a look at the ovaries and see if there are signs of cancer there.
Alison - Yes. I have here in front of me the pelvic organs which includes both the ovaries, the fallopian tube and the uterus or womb. I think you can probably see that there are these craggy, white nodular deposits all over the surface of uterus and also over both the left and right ovaries. It's quite hard to make out where the fallopian tubes are because they're completely encased and embedded in these two tumour masses surrounding the ovaries. I am certain that what we're dealing with here is a primary ovarian tumour with metastasis in and throughout the abdominal cavity and ultimately spread to the liver as well.
Chris - So we started today with someone who was found collapsed at home. They died suddenly, that's all we knew. If you could put it all together for us and tell us how you've actually reached the conclusion you have as to what happened to this lady.
Alison - In summary this lady has essentially had a large tumour I would think growing some time in her abdominal cavity, causing abdominal distension. We have massive tumour deposits in her abdomen. These have ultimately ended up compressing and obstructing her bowel so she's developed a bowel obstruction where the contents of the bowel can no longer pass normally through and which has caused her to begin to vomit. This vomiting has ultimately been so much that she has actually been unable to breathe and vomit at the same time. So she's ended up breathing in a large amount of the gastrointestinal content into her lungs and that has caused her acute and sudden death.

45:06 - How long would it take to wipe all trace of man from Earth?
How long would it take to wipe all trace of man from Earth?
We put this to John Nudds, University of Manchester, Senior Lecturer in Palaeontology Thinking first in terms of archaeological timescale if the human race were to become extinct tomorrow then our buildings and roads would gradually decay and possibly within a hundred or hundreds of years many buildings would start to collapse. The sturdier stone built buildings would stand a lot longer than this as we know because we still have Greek Temples and Egyptian pyramids with us today. If we think in terms of those ancient civilisation sit will only be a few millennia before our city would firstly be overcome by vegetation and then would be buried by silt and sediment. If you consider the fabrics used in modern day construction: reinforced concrete, plastics etcetera these would certainly survive the burial for at least as long as the two million year-old stone tools dating from the early humans from Africa, for example. If we think in terms of a geological timescale - this country and indeed most of Europe has been under the sea for a much greater period of geological history than it has been land. The one thing we can be certain of is that sea levels will rise again and this country will be flooded once more by shallow sea and then all of our cities will become deeply buried by marine sediments. Over geological time, over millions of years they'll be preserved in a rock stratum in just the same way that dinosaurs are preserved in rock strata from 65 million years ago. When we consider that the oldest fossils we have on Earth are 3 and a half billion year-old single-celled microscopic, soft-bodied bacteria. If such tiny and delicate organisms can survive for that long then certainly the robust skeletons of Homo sapiens can survive for similar timescales. In actual fact organisms that live in the sea are much more likely to be fossilised than organisms like ourselves that live on land. So human fossils will always be rather scarce. We know this already because although hominids have been around for say five million years the actual numbers of fossil human skeletons is very low. Certainly some of us will be fossilised and we will survive buried in rock strata. To answer the question, when the human race does eventually become extinct, as it certainly will, although evidence of our existence will disappear from the Earth's surface relatively quickly - say within a few millennia - evidence of our existence will survive buried at depth probably for as long as the planet survives.
Why do some drugs work against more than one disease?
We put this to Professor Adrian Newland:
Adrian - In diseases such as Wegener's which is an autoimmune disease it's the immune system, the lymphocytes that actually cause immune damage. CamPath just removes those whatever the disease and will deal with that.
Chris - It'll take away the cell that is causing the disease so the disease gets better.
Why does blood not clot when it’s in a surgical drain?
We put this to Professor Adrian Newland:
Adrian - It may eventually clot but at the operation site blood gets activated so the clotting factor's actually get stimulated and removed so the blood is able to clot and it will build up around the wound and cause damage and prevent healing. It's sucked out. Chris - When you say clotting factors, Adrian, what actually are they?
Adrian - They're little cells called platelets but also chemicals within the blood called clotting factors.
Chris - How do they work?
Adrian - They work by becoming activated by raw tissue and they form a little spider's web that brings the blood together. Chris - And it grabs blood cells, presumably? It forms this meshwork and you don't bleed any more. If you've got oozing through that just plasma and things what Thomas might have been seeing in his drain was just plasma minus these things that have already been removed?
Adrian - Yes. It might have been exudate that oozed out and was being sucked away.
How many calories do you need to replace a pint of blood?
We put this to Professor Adrian Newland:
Adrian - About 650 calories, which I'm reliably informed is 3 Mars bars.
Chris - Why would it take energy to replace blood? Adrian - Anything that develops tissue requires energy.
Chris - So what you're saying is you just need to put the energy back in.
- Previous Carbon Capture and Forest Fungi
- Next Ageing










Comments
Add a comment