News from the NCRI Conference
Interview with
Kat - I'm here at the NCRI conference, that's the National Cancer Research Institute which is an organisation which brings together all the funders of cancer research here in the UK. That's people like the government, charities all sorts of organisations that are funding cancer research. The conference is really a fantastic opportunity to showcase what's going on in the world of cancer research. We've got everyone from people doing the really fundamental lab research. We had a talk this afternoon from Professor Tony Kouzarides from Cambridge University who's looking right at the sort of molecular post-it notes that are put on our DNA that are important in cancer. Right now we're sat above the lecture theatre and there's someone talking about the importance of dying with dignity when people come to the end of their journey with cancer. There's going to be everything from the very basic research through to the much more quality of life, patient care areas.
 Chris - What's the problem with the UK allegedly not doing so well with the cancer stakes compared with the rest of Europe?
Chris - What's the problem with the UK allegedly not doing so well with the cancer stakes compared with the rest of Europe?
Kat - Exactly. The first lecture today was from Professor Michel Coleman from the London School of Hygiene and Tropical Medicine. He's one of the world's leading epidemiologists. That's someone who studies the statistics and the populations to do with cancer and he was pointing out there have been a lot of studies. These Eurocare studies that have shown that Britain pretty much is one of the sick men in Europe. In terms of football league tables we're drifting towards the relegation zone. This is happening for a number of reasons. For a start the Eurocare studies are using relatively old data. In fact, here in the UK around the year 2000, 2002 we brought in a cancer plan. We are turning around what we're doing but it has shown that the UK has been falling behind. It's not actually what people think. It's not about access to drugs. It's actually really to do with early detection. That was one of the most interesting results hat he showed. When you look at five year survival rates across Europe (this is the standard bench mark that people use for how many people survive that long). If you take out from those statistics all the people who die from cancer within a year, that's people who die from very late/very advanced tumours, if you take those people out of the equation Britain comes back in line with the European average. This tells us that in fact in Britain our major problem is diagnosing cancer early.
Chris - Why is that?
Kat - There's a number of reasons. It's obviously a problem with just educating people. We need to get more information out there about what the symptoms of cancer are and that people should not just get the stiff upper lip and think it'll probably go away if I ignore it. Go to the doctor. There's also an issue with educating the GPs as well to spot when someone presenting with certain symptoms may have cancer. You'd think well cancer is a relatively common disease but actually GPs may only see six to ten patients a year who actually do have cancer in a list of 2-3000 patients. It's not really that common for each GP so we need to do more in education for GPs and the public. Also more in things like CT scanning, MRI scanning to try and get cancer detected as early as possible.
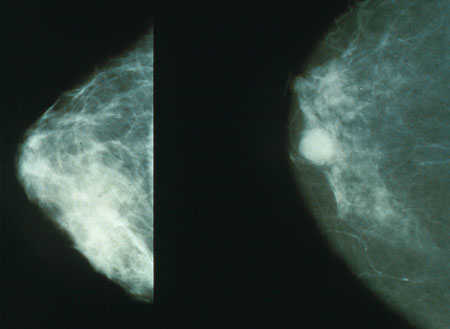
Chris - Also in the news this week is a story about how computers can help to read mammograms which might help to bring out the prediction and detection rates.
Kat - Exactly and this ties in to the whole early detection thing. In the Uk we have a fantastic system of breast screening run by the NHS and it does save thousands of lives. It invites all women in their fifties from fifty to seventy to go for a mammogram every three years. Every mammogram is read by two doctors; two radiologists look at it, look for any dodgy spots and decide whether to call the woman back or not. Now what these researchers, led by Professor Fiona Gilbert at the University of Aberdeen, have shown is that you can use one doctor and a computer-aided detection system. How this works is the computer system scans through the mammogram, spots anything that it thinks looks suspicious and then the doctor looks at it and goes, ' Yep, that looks dodgy...no, that's just an area of fluff or whatever.' Then you only need to have one doctor's time per mammogram. Basically you're holding the workload for doctors. This is really important because in some areas of the country we're seeing screening - the interval of screening is meant to be 3 years - but we're seeing it drift out to three and a half, four years. There simply aren't the resources. This could be a really great way to get more women screened and to help ease the pressure on screening services.
Chris - Which would be very good for affecting that diagnosis detection problem.





Comments
Add a comment