Cancer mood control, and birth products blocking pain
This month, signs that cancers communicate with the brain to alter mood, why antibodies are unreliable in research, evidence that social training can cut stress and boost brain volume, and agents derived from birth products that suppress inflammation and kill pain...
In this episode

00:39 - Cancer converses with the brain to alter mood
Cancer converses with the brain to alter mood
Paola Vermeer, University of South Dakota
People diagnosed with cancer also frequently develop mood disorders like depression, but sometimes before they even know they have the disease, ruling out just having cancer as a cause. But could the reason be that their cancer is in conversation with, and manipulating their nervous system? Paola Vermeer is a researcher at the University of South Dakota. She’s found that developing cancers seem to form associations with nearby nerves, and strike up a relationship. The nerves can grow into the tumour, which can “listen to” and respond to the signals issuing from those nerves; but even more intriguing is that the cancer seems to be sending messages back to the brain via those nerves, altering brain activity and chemistry, and therefore potentially also mood. She’s just published a paper in the journal eLife documenting how this seems to happen. It might, she argues, lead us to new ways to approach the management of cancer…
Paola - So we've known that tumours actually can infiltrate the nerves and that's, associated with a poor prognosis for many cancers. But what we're now learning is that it happens the other way around, that the nerves can actually infiltrate the tumors as well. They are two very separate processes. So when the tumour contacts the nervous system, it can utilize that as almost a roadmap to get to different parts of the body and metastasize. So, it's a route for metastasis, but when the nerves infiltrate the tumours, they can actually release factors that further, promote increased proliferation of the tumour and allow it to grow.
Chris - So it's almost like in the same way as the nerve would talk to a target organ in the body, like a muscle, it can talk to the tumour and provoke behavioural change on the part of the tumour?
Paola - Oh, absolutely. We've started to define some of these molecules that are used in these conversations. So there's actually talk from the nerves to the tumors and then from the tumors back to the nerves. It's a very active communication where the two entities impact each other.
Chris - And what about higher centres? What about, if you have a sensory nerve contacting a tumour and obviously the job of a sensory nerve would normally be to relay information centrally up to the brain. Does that actually get reflected in a change in behavior then?
Paola - Yes, absolutely. And we were very intrigued by this because cancer patients really suffer a decline in their mental health. And we can study this by looking at behaviour in mice where we implant tumours. So we saw that the brain was changed and the mouse behaviour was also changed.
Chris - When you say the brain was changed, what did you actually see?
Paola - We saw that the brain regions that were connected to the nerves in the tumour, had a very high activity. They were firing a lot more than the same regions of the brain from a non-tumour bearing animal.
Chris - How was that reflected in behavioural change?
Paola - The behavioural tests that we use were really reflecting the wellbeing of the animal. And so their behaviors for those animals that had tumors went significantly down as the disease progressed. So they wouldn't make a good nest or they wouldn't eat a cookie because they were essentially depressed.
Chris - And this is not just because tumours are painful, because as we know when when you have a tumour growing invasively through various tissues, that is extremely uncomfortable. It wasn't just that in these animals, they're in pain, that's why they withdraw socially?
Paola - No. In fact, we tested that, and we had a group of mice that we gave a tumour to, but then we treated them with a medication for their pain and that did not fully restore their normal behaviour. So it's not only pain information that is being relayed to the brain, there's more to it than just that.
Chris - And what about different types of tumour? Because some are more nerve-like in their behaviour and the sorts of tissues of origin and the things they make, the tumours themselves. So would you expect that some tumours are probably going to have these sorts of effects to a greater extent than others?
Paola - Yes. And as you said, the location of the cancer can really dictate not only the extent of how many nerves infiltrated, but also what type of nerves. So, all the tumours that we've looked at so far are innervated, but the types of nerves could be different and therefore the influence of the nerves on the cancer could also be different.
Chris - What do you think this tells us then? Does this sort of show us a way that we should manage cancer differently or does it open up different avenues for management?
Paola - Absolutely, It tells us that so far all the cancer medications that we have completely ignore this nerve component of the tumour. So that isolates the nerves as a therapeutic target. And since we know some of the molecules, we can design drugs to target them. But it also tells us that beyond the local tumour, we need to consider what the connections to the brain are and how we can therapeutically mediate changes in behaviour in cancer patients as well.
Chris - And looking at it the other way around, if you make the person's mood better, does that affect the behaviour of the tumour?
Paola - We haven't tested that directly, but given the bidirectional nature of these communications, I would expect that yes, if you can change the neurons in the brain and the behaviour that should have an impact on the tumour itself.
Chris - Why has no one looked at this before?
Paola - The understanding that nerves are in cancers is, is relatively new, as surprising as that sounds. So we are just at the early stages of understanding, not only that the nerves are there, how are they getting there? What are they doing? And what other neural components are they connected to? It's a very young field.
06:36 - Unreliable antibodies
Unreliable antibodies
Rick Khan, Emory School of Medicine, & Peter McPherson, McGill University
Apart from winning a Nobel prize for their discoverers, and along the way enabling millions of women to tell whether they’re pregnant, antibodies have been revolutionary for research. We use them therapeutically to detect and treat diseases; and we use them for research all the time to activate and block cell signals, and to reveal microanatomical features in histology. We’d like to think that we can rely on them as rock solid science: doing what they say on the tin. But, as Rick Khan, from Emory School of Medicine, and Peter McPherson, from McGill University, argue, as the industry has expanded, the detail, breadth and quality of the characterisations being carried out on the antibodies routinely used to drive research has nosedived. Scientists, they highlight, tend to take as read that if another practitioner has used and published work based on an antibody, then it’s probably okay for them to use it too; yet the actual performance in the context they’re seeking to use it may never have actually been ascertained. Once the implications for the reproducibility of research and integrity of our discoveries are appreciated, it’s impossible not to feel a shiver go down the spine. Rick first…
Rick - Antibodies are incredibly valuable and useful reagents. Initially they were developed in researchers lab and then shared with their colleagues. Over time this became such a big important field that companies began to distribute them and, as a result, work on demonstrating their utility and their proper use fell by the wayside. And this resulted in a wide scale problem of poorly characterised antibodies. And as a result, using them improperly or overly interpreting their data leading to science problems and or just spending money on an antibody that didn't work and they just waste money.
Chris - Indeed, because you highlight the scale of the problem in the manuscript you've written. Because you point out that a couple of decades ago we had a few thousand antibodies and now we've got north of 6 million.
Rick - Right. And it's increasing rapidly as a result of new technologies.
Chris - And there's just no kind of industry standard that says we have evaluated each of these and these are its operating parameters. This is what you can rely on, this is what you can't, this is the uncertainty, that's just not done for some of these antibodies.
Rick - One of the real problems here is they're such valuable reagents. They're used in a variety of different assays. So each use needs its own verification. And so for a company to sell an antibody and to do all the verification themselves, they'd be losing money.
Chris - Presumably then that means that there's going to be a trickle down effect. Because if I publish a paper having used one of these antibodies, any inherent shortcomings in that antibody will be reflected in my science. I've done good science. But the data may be flawed.
Rick - Correct.
Chris - Well what's the scale of that problem then? That sounds huge.
Rick - It is huge And part of the problem is the people using them don't always appreciate that. When you go to buy anything, you assume the seller has done proper characterisation and know that what they're selling you is legitimate. That is not true with the antibodies because the company's distributing them or simply the middleman distributing them.
Chris - What's it going to take to sort this out, Peter?
Peter - What it's really gonna take is more of a fundamental cultural change. We need to make the scientists understand that the reagents that they're using are not always up to the professional contemporary standards and they're using reagents that simply aren't validated.
Chris - Do you think that phenomena like this are what underpin parts of the reproducibility crisis that have been documented in certain areas of science.
Peter - The reproducibility crisis is real and we believe antibodies are a major contributor to that.
Chris - How cognisant, Rick, do you think scientists but also industry are of this problem and the scale of it?
Rick - That's a great question. <laugh>. It's hard to judge. I have run two different antibody core facilities where we generate and work with researchers and from that work it was clear very talented, very smart scientists simply don't understand the scope of the problem and they assume if we generate an antibody for them, it will do everything they want it to do. And it simply does not. You know, it costs money whether the companies do it, which they don't, or the researcher does it. It costs time and money to do that work. And too many of us are too eager to get on with the interesting experiment. And so we're not training our folks enough to realise, 'hey, you've got to first convince me in the world that that antibody is doing what you think it's doing in that particular usage.'
Chris - I suppose we've also got, Peter, a problem, both a forward direction problem but also a reverse direction problem, which is if we discover or if we implement some evaluation of antibodies and we discover, which inevitably we will, that some are unreliable for the use we're employing them for, we're then going to undermine the evidence base going backwards in time and cast doubt on publications backwards in time. But we're also then potentially going to cause problems going forward. Where do we go from here? Because we're relying on dodgy data from yesteryear, but also how does that inform how we change things going forward to do the next set of experiments?
Peter - Correct. So we looked at this and we've looked at what criteria do the scientists use. And one of the criteria that scientists use is, has this antibody been used in a previously published paper? And it turns out that's not a very good criteria for judging whether you should use an antibody or not. So you're absolutely right. It's a problem that propagates, a scientist looks at a paper, says, 'well this other scientist uses antibody, they used it in their paper, therefore I think that it must be a good reagent to use. I'll use it in my paper.' And it turns out it's really not.
Chris - The problem is if we say, well look, we've got this reproducibility crisis, so we're going to repeat experiments if we repeat experiments and use the published method that someone went through to reproduce their data and we use the same reagent with the same inherent flaw, we're going to get the same flawed outcome.
Peter - Exactly correct. And this is part of this cultural shift that's required to not think that just because an individual has used this antibody in a published manuscript or published study, that you can work on the assumption that it's the right reagent, it's a business model and a cultural model that needs to be changed and how to do that? These are not trivial questions, this is stuff that's been going on for a very long time. And part of what our initiative is trying to do is trying to figure out how to push the cultural change as much as the scientific change.
Chris - What do you think then, Rick, some kind of level from the funders down that says you have to use antibodies that have been approved in the following way or validated in the following way. So in the same way as we had a big shift towards open access publishing, for example, led by funders. Do you think that funders, and possibly also journals, should be more rigorous in this sort of thing and that's how we effect culture change?
Rick - That can be a big part of it. I have been in contact with the leadership at several of the institutes in the National Institute of Health, as well as the National Science Foundation, to bring up this issue and to encourage them to encourage change. And the first answer you get is they are not a regulatory body. So on one hand they don't want to take a heavy hand in this because that's not how they see their role. On the other hand, they have been increasingly asking for, when you submit a grant, to have a section where you describe and deal with the reproducibility issues. I think it's now inherent that one potential solution or partial solution is for reviewers of grants and papers to raise this issue and make sure that the folks doing the work understand it and will appropriately address it. That's really part of the cultural change that Peter is alluding to. I think the funding agencies can do a better job. I should mention also there are some private foundations, disease related and other, that are also doing a great job and they can be more persistent in demanding such work. And just pointing out one, the Michael J. Fox Foundation I think is doing a great job and I think they can be a prototype for others.
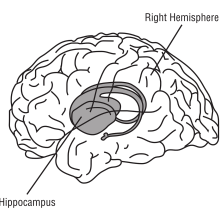
16:00 - Social de-stressing and a brain volume boost
Social de-stressing and a brain volume boost
Sofie Valk, Max Planck Institute, Leipzig
Chronic stress is associated with accelerated ageing and a shrinkage in the brain’s hippocampus, the region concerned with learning, memory and finding our way around. But is the converse also true, and can we de-stress individuals and help to reverse these changes with behavioural training? That’s what Max Planck, Leipzig, scientist Sofie Valk wondered when she recruited a group of adults who were tested for stress hormones and underwent brain scans at baseline and then again after a period of social training aiming to cut stress. And the answer appears to be yes: levels of the stress hormone cortisol fell, and the MRI brain scans showed a small volume increase in one region of the hippocampus…
Sofie - We wanted to understand how mental training impacted brain structure, focusing on the hippocampus and how this could relate to stress reduction. The mental training was very specific. So it was about training social skills, either by targeted interaction with others and also forms of meditation. So mental practice over three months.
Chris - How do you know that people who took part in this actually learned anything through the training?
Sofie - Well, we took a lot of questionnaires before and after they did training and we also looked at their brains and also at other physiological markers such as, in this case, cortisol.
Chris - Tell us about how you looked at their brain.
Sofie - So we used a magnetic resonance imaging and we looked at how the grey matter of the brain was shaped, but also how resting state connectivity, so the functional connections when you don't do anything, relate to other regions in the brain.
Chris - Presumably you did that at baseline, then you give people the intervention and then you look again. And where does the measuring the stress hormones come into this? The cortisol that you mentioned?
Sofie - This was done during a week of measurements where people were asked at different parts of their day to measure their saliva. Cortisol was gotten out of the saliva. This was the process to understand how it changes over the day, then used as a marker of stress.
Chris - And again, is that done on the subjects before they have any training and then after they complete the training to see if there's any effect?
Sofie - Exactly. Exactly.
Chris - And what did you actually find then? So when you give people these training exercises, first of all let's think about their brain. How does their brain change?
Sofie - Their brain changes in various ways. In this case, we looked at the hippocampus specifically and we looked at the different subfields in the hippocampus. And here we looked at the volumetric changes. So whether the hippocampus subfield got bigger or smaller. And then we did a statistical analysis to see if training had a certain effect on the volume of these subfields. So in this case, we saw a specific change following social effective training. So people learning to be more compassionate and empathetic in the CA123 subfield, but not in the other subfields.
Chris - How big was the difference? Because that's quite striking that you give people this short period of training and you see that reflected in literally a volumetric change in the brain. But is it a big change?
Sofie - No, because you would get a headache. No <laugh>. So it's a very, very subtle change. But based on statistics, we find that overall there's a subtle increase in volume, maybe one millimetre.
Chris - Is that on both sides of the brain, Sofie, or does it tend to be on one side preferentially.
Sofie - I think we had no hypothesis about there being any hemispheric differences. So actually I was rather happy to see this happening consistently in both hemispheres because it gave me more faith in our findings.
Chris - And in both men and women. Or was there any kind of sex bias?
Sofie - We didn't look at sex bias. Other people have done it. And of course there's a whole literature also on the impact of hormones on hippocampus and thinking about menstrual cycles. So a good hypothesis that there could be differences between sexes. But here we didn't look at this specifically.
Chris - What about the cortisol? How did that change?
Sofie - So we saw that there was actually a reduction in cortisol, specifically after social effective training, meaning that people got less stressed.
Chris - Why is it important to consider both the cortisol and stress level than what's going on in the hippocampus though? How do you marry those two things together and what's the relationship?
Sofie - The hippocampus is full of glucocorticoid receptors. It is the key region that has been implicated also in animal studies in being very susceptible to stressors and specifically cortisol.
Chris - So in other words, if you have high cortisol, you what damage or change or reprogram the hippocampal region.
Sofie - Exactly. That is the idea, yeah.
Chris - And so why would the training affect that axis?
Sofie - Well, because if you then would reduce stress, the idea would be that this would then have a positive effect on the hippocampal integrity and structure.
Chris - So which way round do you think it is? Do you think that the training makes people less stressed and therefore their cortisol levels are lower and therefore their hippocampus is allowed to grow bigger because it's not being so stressed? Or is it that the training makes the hippocampus bigger and it makes cortisol go down and the two aren't connected?
Sofie - That's a very good question. So I think it's a little bit of both because the hippocampus is obviously not only related to stress, but also to memory and other functions. It would be a very interesting follow up to understand what is actually the sequence of events. But even though we took our measurements before and after the training, it's very hard to disentangle both processes. So at the moment, we don't know. Possibly if you reduce stress and thus have less cortisol, you kind of protect the hippocampus. Hence it gets a little bit bigger.
Chris - What's the take home message then off the back of this study?
Sofie - That if you are part of a mental training or if you take a mental training that reduces your stress levels, this may impact positively. Like it may impact the size of your hippocampus, especially the cornu ammonis.
Chris - So, basically, I could be a memory marvel, if I had a quiet life?!
Sofie - Maybe. At least the chances could be better. But of course, stress is so complex. It's not that a totally quiet life would only have beneficial effects. So theoretically, a little bit of stress may also not be that bad. But this is also something that we didn't study in this work, and I think the biggest take home is that stress impacts your brain and by producing levels of stress, you may also protect your brain. Again, this is not something that we looked at, but at least it suggests some relationship between a behavioral intervention, stress physiology, namely cortisol and the anatomy of the brain.

23:17 - Placental products help healing and block pain
Placental products help healing and block pain
Scheffer Tseng, BioTissue, & Yun Guan, Johns Hopkins
And now to an interesting study from Yun Guan, at Johns Hopkins, and Scheffer Tseng, from the company BioTissue. They’re pursuing the intriguing observation that human birth products - meaning components in the placenta, amniotic membranes and the umbilical cord - seem to have powerful pain-killing and pro-healing effects. And now they think they have tracked down one of the chemicals responsible, a component called HC-HA/PTX3, which appears to manipulate cellular ion channels, cutting down pain transmission and inflammation. And it potentially has the great virtue that it can be administered only where it’s needed rather than delivered systemically like most painkillers. Scheffer Tseng first…
Scheffer - The birth tissue is quite effective in delivering anti-inflammatory and the antiscarring actions. We also observe that patients with this treatment experience a pain reduction. So I was so eager to find out what could be the action mechanism.
Chris - Yun, can you just clarify though, when we're saying people get pain reduction effects from birth products, what does that mean?
Yun - So,Chronic pain and post-surgical pain is big problem. So they need to have a better treatment. Currently, the opioids is the main treatment, but have a lot of side effects. We're eager to find new treatment. What we found is that in a post-surgical pain model, using this human birth tissue product, it produce beautiful pain inhibition without causing side effect.
Chris - But what are these birth products that we're referring to?
Yun - The birth tissue products comprise the amniotic membrane. So these contain different layer of cells that can secrete a lot of bioactive molecules. Some of these molecules have beneficial effect. Like we mentioned, anti-inflammatory, and also there's anecdotal evidence from clinical observations that patient feels pain relief
Chris - Scheffer. How do you actually make the preparations then?
Scheffer - Birth tissue used to be regarded as a medical waste and we were the first company bringing the birth tissue for the commercial use. In brief, after consenting the pregnant mother, through a elective caesarean section delivery we are able to obtain the placenta from which we then able to retrieve both amniotic membrane and umbilical cord. We process that into a membrane, a sheet, so that can be used in the surgical setting to cover a wound, but also we can turn that into a powder so that that can be injected into deeper tissues.
Chris - And is this viable tissue or has this been rendered non cellular? So you remove all the cells and just produce a sheet of material that doesn't have any living cells in it?
Scheffer - Yeah, we kill the living cells first. The product we prepare consists of the remaining tissue components, all the extracellularmatrices, the different growth factor and cytokines present in the tissue.
Chris - Right. And Yun, what did you do with them?
Yun - To test these birth tissue products on pain, we use an animal model induced by cutting the handpaw of little mice, mimicking this post-surgical pain conditions. These animal shows pain behaviour like we feel after surgery. We apply this birth tissue product before or after this surgery, and then we measure the animal's pain behaviour and we notice a significant improvement in the pain after surgery.
Chris - Is it just the behaviour or can you measure the nervous system and show that actually there is a reduction in nerve activity or is it just that they think they're feeling less pain?
Yun - That's a great question. That's actually one of the first major finding of this paper because although there's some clinical observation, some patient report pain reduction, we don't know what is the mechanisms. We don't know whether these human birth tissue product can really directly inhibit the neurons, which are the cells that mediating this pain signal from the peripheral to the brain. So after we confirm that animal's pain behaviour is reduced by this treatment, we recorded the neurons transmitting the pain signal from the peripheral to the spinal cord and the brain. And surprisingly we saw significant inhibition of neuro responses by this treatment.
Chris - Do you know what it is about the treatment that does that? Because if you've just made a mixture of stuff from birth products that you've ground up and rendered safe, that must be a whole cocktail of material. So do you know what in there is doing this?
Yun - Absolutely. I think that's a great question and also is what Dr. Tseng and we are trying to figure out. Luckily in addition to using this cryo-preserved human birth tissue product called flow, Dr. Tseng's company also can now purify a water soluble abstract from this human birth tissue product and they called this HC-HA/PTX3. And this only exists in the human birth tissue during pregnancy. And early evidence from Dr. Tseng's group in other indications suggesting this HC-HA/PTX3 may be ne of the most important bioactive component in that human birth tissue product, but we still don't know whether this compound also mediate the pain inhibition.
Chris - So you haven't, for instance, injected just that compound back into your animals to see if you can mimic the pain killing effect of the original product just with that alone.
Yun - So that is the next stage of this study. So after we confirmed the pain inhibitor effect, then we repeat the study by just giving this purified compound at HC-HA/PTX3 and strikingly this purified compound itself, also mimic the pain inhibitory effect of the human burst tissue product and also produce a robust neuronal inhibition on this pain transmission.
Chris - Have you worked out how the cells are seeing this? In other words, how's it exerting its effect? Do the neurons directly respond to it or does it have some kind of modulating effect on the wound and that then affects the nerve cells? Do you know downstream how it works?
Yun - Right. So in order to address this very important question, what is the mechanisms of action, we found that this compound can produce an inhibition on the iron channels on these sensory neurons that are not important for pain, such as sodium channel and calcium channels.
Chris - And is the amount of pain reduction clinically meaningful? So in other words, how much morphine would I have to give myself to get the same effect as giving me some of this stuff? Are they analogous or is this much, much less potent?
Yun - This is a very difficult question to answer because you have to really compare these two drugs side by side in terms to understanding the efficacy and potency. But I think that advantage of these human birth tissue products, specific to post surgical pain is we applying these treatment locally at the wound. So where the pain is generated by the sensory neurons, we can directly inhibit this neuro activity. In addition, we also observe these anti inflammatory action compounds. So not only in hip pain, but we also can produce facilitated wound healing and reduce inflammation. Morphine like that does not have this beneficial effect.










Comments
Add a comment